A Nipah virus outbreak was recently reported in the Indian state of Kerala, where there were 6 confirmed cases, including 2 deaths. India has previously seen 4 odetroit lions jersey ohio state jersey micah parsons jersey 49ers jersey College Football Jerseys custom made football jerseys Ohio State Team Jersey fsu football jersey College Football Jerseys Ohio State Team Jersey custom made football jerseys OSU Jerseys ohio state jersey micah parsons jersey fsu football jerseyutbreaks of the Nipah virus between the years 2001 and 2021, and the most recent outbreak brings the total to 5. Few infectious viruses that have recently emerged hav
reebok osuska gros fitness
nike zoom structure 21 black
Combinaisons roll on jade
collagen booster cream rich
prada schuhe 2017
bakugou uniforme ua
isp 6 pin
czc redukce na sluchátka
mercatino canne da pesca usato amazon
starbucks 2000 termos
lagan gáz főzőlap
andre johnson houston texans jersey
houston texans andre johnson jersey
zalando levis t shirt
lego stargate sg 1
e attracted as much attention and concern as the Nipah virus. This elusive virus, which was named after the Malaysian village of Sungai Nipah where it was discovered in 1999, has raised concerns because of its high fatality rate, the possibility of human-to-human transmission, and its origins in the animal realm. This article delves into the world of the Nipah virus, examining its traits, background, current research, and effects on global health.
The Emergence of Nipah Virus
In 1999, the Selangor state of Malaysia saw the first appearance of the Nipah virus. Due to the similarity in clinical symptoms, such as fever, headache, and neurological problems, it was initially misdiagnosed as Japanese encephalitis. The high mortality rate linked to these instances, however, caught the attention of epidemiologists and virologists, which resulted in the identification of a novel disease.
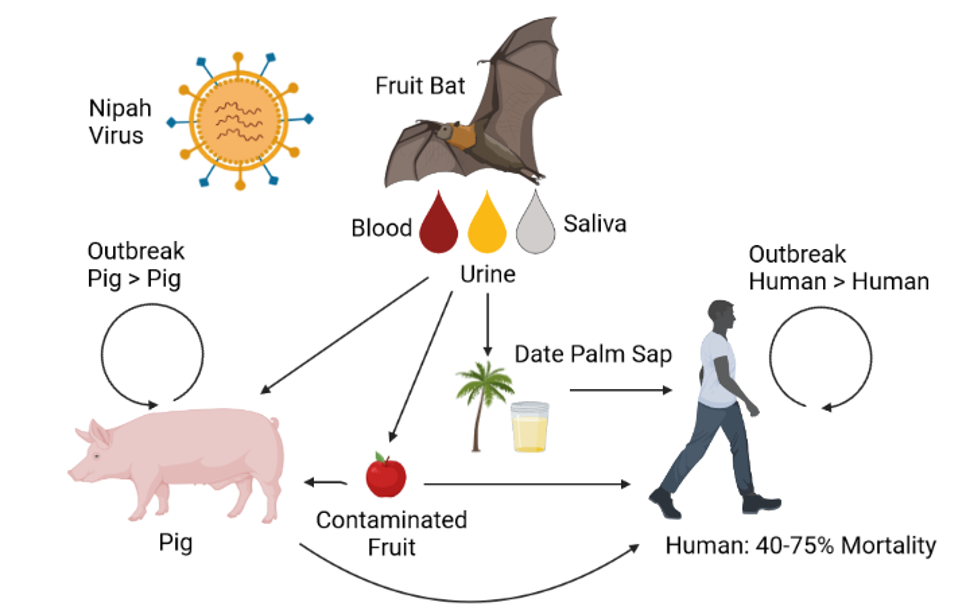
Further research established that humans likely contracted the Nipah virus from fruit bats of the Pteropodidae family, the virus’ natural reservoir, by ingesting tainted date palm sap. This was the first time a virus had spread from bats to people via an intermediary host.
The Nipah Virus Genome
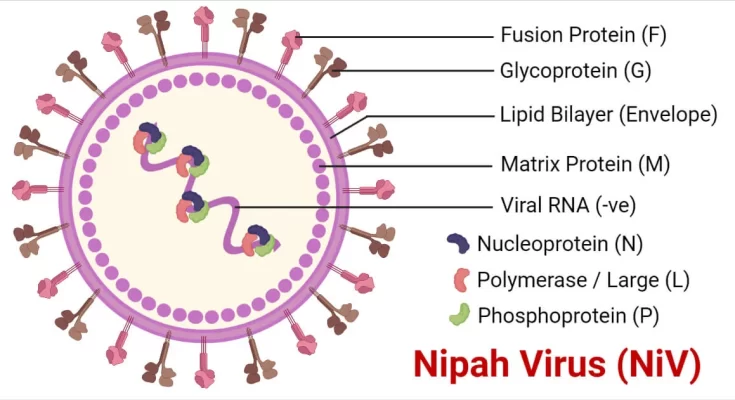
Scientists have closely examined the genetic structure of the Nipah virus for a better understanding of its complexity. Along with the Hendra virus, the Nipah virus belongs to the Henipavirus genus. Both viruses are regarded as lethal zoonotic diseases and have genetic similarities.
An RNA with a single strand called a negative-sense strand makes up the Nipah virus genome. This protein encodes a number of proteins, including the fusion protein, which is essential for the virus’s ability to enter host cells. In order to comprehend the pathogenicity of the virus and create viable therapies, researchers are closely investigating these genetic components.
Dynamics of Nipah Virus Transmission
Direct contact with infected animals or their secretions is the main way that the Nipah virus spreads to people. Pigs were used as intermediate hosts in Malaysia, where the Nipah virus was first discovered, and intimate contact with these animals led to human infections.
A major worry is that the Nipah virus could spread from person to person, especially in outbreak situations and medical facilities. There have been documented cases of human-to-human transmission, frequently in intimate and extended contact with infected individuals, even though the predominant mechanism of infection is through direct contact with infected animals or their secretions, such as their urine or saliva (figure 1).
The majority of cases of this secondary transmission are seen in healthcare settings when caregivers and healthcare personnel may come into touch with infected patients’ blood, respiratory secretions, or other bodily fluids and get infected themselves. In addition, close, unprotected contact with an infected person can result in transmission within families or communities, particularly in the latter stages of the illness when virus levels are high.
Clinical Presentation and Diagnosis
An infection with the Nipah virus can result in a variety of clinical presentations, from minor respiratory symptoms to serious encephalitis. In extreme situations, the virus may result in coma, convulsions, and acute respiratory distress syndrome (ARDS). The virus’s incubation period, which spans from 4 to 14 days, makes it difficult to diagnose the disease early on in its progression.
The significance of laboratory diagnoses is highlighted by the lack of distinctive clinical characteristics that set Nipah virus infection apart from other respiratory infections. At the moment, serological assays and molecular testing like polymerase chain reaction (PCR) are the gold standard for diagnosing the Nipah virus. To facilitate quicker case identification, particularly in resource-constrained situations where outbreaks frequently occur, rapid diagnostic assays are being developed.
Nipah Virus Outbreaks: A Global Perspective
Numerous nations, including Bangladesh, India, Malaysia, and Singapore, have experienced Nipah virus epidemics (Figure 2). Significant morbidity and mortality have resulted from these epidemics, with case fatality rates frequently exceeding 40%. The Nipah virus poses a serious risk to public health because of its recurring nature and potential for human-to-human transmission.
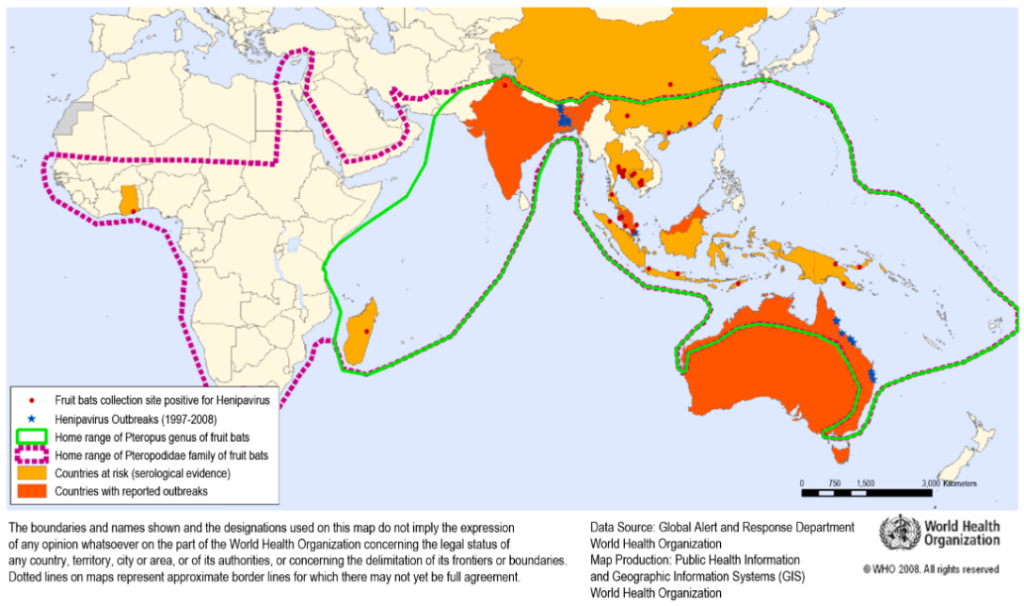
Fruit bats are thought to be the main Nipah virus reservoir in Bangladesh and some areas of India. Human transmission in these areas has been linked to the consumption of infected fruit or date palm sap. The virus can survive in bats and has the potential to spread to human populations, which emphasizes the necessity for continued monitoring and protective measures.
Prevention and Control
Since there are no specific antiviral medications to treat the Nipah virus, prevention is still the best course of action. Important safeguards against Nipah virus infection include:
1. Avoiding Exposure: It is important to limit contact with sick animals, bats, and their secretions. It is advised to avoid the consumption of raw date palm sap and fruits with bat bites or scratches in endemic areas.
2. Infection Control: To avoid nosocomial transmission in healthcare settings, strong infection control procedures, including the use of personal protective equipment, are crucial.
3. Immunization: Several unproven vaccines against the Nipah virus are being developed and have shown promise in preclinical research. These vaccines might be essential for stopping further outbreaks.
4. Public Health Surveillance: For early diagnosis and response, surveillance systems that keep an eye on both human cases and potential reservoir populations are essential.
Human-to-human transmission of the Nipah virus must be prevented in order to contain outbreaks. Here are some crucial safety measures:
- Isolation of Infected Patients: In order to prevent interaction with others, healthcare facilities should immediately isolate anyone who has a suspected or confirmed Nipah virus infection.
- Use of Personal Protective Equipment (PPE): To reduce exposure to bodily fluids, healthcare staff should wear the proper PPE, such as masks, gowns, gloves, and eye protection, when caring for infected patients.
- Strict Hand Hygiene: After any interaction with patients or possibly contaminated materials, healthcare professionals and caregivers must regularly wash their hands with soap and water.
- Implement stringent infection control procedures in healthcare institutions, including the cleaning of surfaces and medical equipment, to avoid the contamination of the environment.
- Reduce Close Contact: Especially in the later stages of the illness when virus loads are higher, family members and caregivers should reduce close contact with those who are infected.
- Safe Burial Procedures: Adhere to safe burial procedures, which include staying away from customary procedures that require close contact with the corpse because the virus may still be present there.
- Encourage Respiratory Hygiene: To lower the risk of respiratory droplet transmission, encourage respiratory hygiene practices including covering the mouth and nose when coughing or sneezing.
- Identify, monitor, and confine anyone who has had frequent contact with sick patients in order to stop the spread of the infection if possible.
The mysterious and potentially fatal Nipah virus continues to be a threat to world health. The need for continued research and readiness is highlighted by its capacity to generate epidemics with significant mortality rates, its complicated transmission dynamics, and its wildlife origin. In order to avoid and lessen the effects of the Nipah virus on human populations, healthcare institutions, governments, and communities must collaborate as researchers try to understand the virus’s secrets. By doing this, we can strengthen our defenses against the looming threat of newly developing infectious diseases.
By: Santhushya Hewapathiranage
References
- Chua, K. B., Goh, K. J., Wong, K. T., Kamarulzaman, A., Tan, P. S., Ksiazek, T. G., … & Lam, S. K. (1999). Fatal encephalitis due to Nipah virus among pig-farmers in Malaysia. The Lancet, 354(9186), 1257-1259.
- Chua, K. B., Bellini, W. J., Rota, P. A., Harcourt, B. H., Tamin, A., Lam, S. K., … & Rollin, P. E. (2000). Nipah virus: a recently emergent deadly paramyxovirus. Science, 288(5470), 1432-1435.
- Clayton, B. A. (2016). Nipah virus: transmission of a zoonotic paramyxovirus. Current Opinion in Virology, 16, 120-126.
- World Health Organization (WHO). (2018). Nipah Virus Infection – Guidance for Infection Prevention and Control. https://www.who.int/csr/disease/nipah/infection-prevention-control/en/
- Lo, M. K., Rota, P. A., & Singh, B. K. (2020). Hendra and Nipah viruses: different and dangerous. Nature Reviews Microbiology, 18
- What is Nipah virus? Kerala starts mass testing after outbreak in India –https://www.theguardian.com/world/2023/sep/18/what-is-nipah-virus-kerala-india-bat-borne-outbreak-mass-testing