Whenever an epidemic unfolds, a certain number of deaths are inevitable. But some will go through the disease phase and recover. Another set of individuals live through the infection even without noticing, which is known in other words as the asymptomatic condition. In any kind of infectious disease whether it is common flu or global pandemic COVID-19, all these three scenarios are possible. Then how to decide who will fall into which category? Most of us are aware that personal immunity has something to do with recovering potential. But can the factor “immunity” alone decide one’s health status, within the vast range of being asymptomatic to deadly?
Does an exposure guarantee the disease?
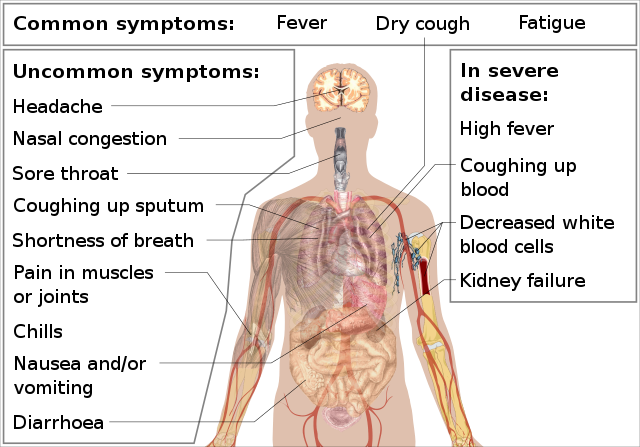
If we are to dig deep into details, it is important to be thorough with terminologies first. The terms exposure, infection and disease hold three different meanings. Exposure to a pathogen generates a probability of developing the infection within your systems, but it does not necessarily mean all exposed individuals will get the infection. Even though the infection begins to spread in your systems it may either give rise to a disease condition or just fade out in an asymptomatic manner. Disease is a clinical state associated with symptoms. The range of which symptoms being mild to severe depends on the damage caused to tissues and the immune system.
When focused on our present calamity COVID – 19, early trends showcased higher susceptibility in elderly people and individuals with chronic lung and heart diseases to severe conditions. Yet, even among the same risk groups (age, gender) significant variability is evident.
These differences have resulted from the interactions of 5 variables.
- Microbial dosage – The first variable indicates the number of pathogenic organisms (viral particles) that get into you through an exposure. When the number is low, our internal defense system takes over and contain the infection. Under such circumstances, the infection will either pass asymptomatically or express mild symptoms. When a heavy viral load is acquired, our defenses are outnumbered by rapid replications leading towards severe consequences.
- Genetic composition – Each individual possesses identical genetic composition. Our genetics come into play when deciding cell surface receptor structures. Usually viruses gain access to host cells via anchorage to surface proteins. Those who lack the relevant surface protein are naturally resistant to the virus.
- Entry route of the pathogen – The pathways through which a virus enters the body matters. Certain viral particles can enter the body along with inhaled air and make way directly to the lungs whereas some can end up in the nasal cavity due to touching one’s face with contaminated hands. Lungs and nose differ in local defenses, hence, activated immune pathways vary creating a major impact on the spread of the virus.
- Virulence of the virus – Even within the same species, viruses differ in strength due to slight variabilities in their genetic matter. When an infection transmits from an individual to individual in a large population, viral genome undergoes changes which will eventually alter the virulence or the capability of the virus to damage host tissues and immune system. Virulence of the virus can significantly influence the possible outcome in a patient as highly virulent strains can cause severe to deadly conditions.
- Immune response – In the battle against any pathogen, the capacity of one’s immune system to contain the infection and fight back is a critically contributing factor for a speedy recovery. Many infectious diseases strengthen our adaptive immune responses and prepare us for a possible second blow. The process of vaccination prior to a disease is a good example of triggering adaptive immune responses. But certain viruses such as dengue makes our immune system susceptible to infection with a different type of the same virus. Facing an infection with a weakened immune system that has fought with some other infection recently can delay our defensive responses and lead to deadly conditions.
Concerning COVID – 19, the probability of reinfection is still debatable. Certain studies suggest that the infection builds immunity in most individuals that last for about one year or more. Yet, studies conducted by South Korea’s Centers for Disease Control and Prevention have encountered several positive cases that were previously tested negative after the infection. Although there are several alternative possibilities to the above-mentioned fact, a great deal of uncertainties about immune responses are yet to be determined.
The above 5 variables appear as different and discrete factors. But in the real-life situation they have combined interactions. Thus, the integrated final picture is far more complicated, and it is impossible to foresee the resulted outcome. These parameters can vary heavily from individual to individual making it even harder to identify the most vulnerable audience. Under the present circumstances where global pandemic COVID – 19 raging across the planet with an exponential death curve, such uncertainties fuel the pandemic’s terror
But to be on the bright side, compared to our past pandemics, modern health care services are equipped with advanced technologies that enable us to combat COVID – 19 better. Even at the moment, a number of vaccines are tested against Covid – 19 worldwide and few out of them have already entered into clinical trials. It lights up hope that together humankind will be able to put full stop to COVID – 19 pandemic in near future.
Story credits –