In a simple but creative experiment, scientists from Harvard Medical School and Technion-Israel Institute of Technology have designed a simple way to observe how bacteria develop resistance to drugs and multiply through increasing doses of antibiotics.
The experiments, published in the Sept. 9 issue of Science, are thought to provide the first large-scale glimpse of the maneuvers of bacteria as they encounter increasingly higher doses of antibiotics and adapt to survive—and thrive—in them.
To do so, the team constructed a 2-by-4-foot petri dish and filled it with 14 liters of agar, a seaweed-derived jellylike substance commonly used in labs to nourish organisms as they grow.
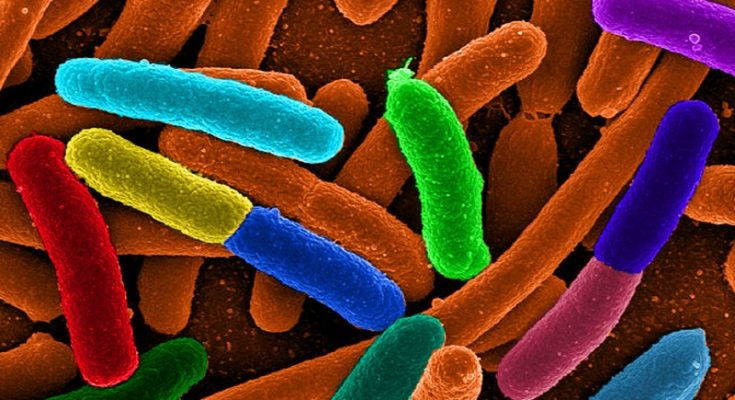
To observe how the bacterium Escherichia coli adapts to increasingly higher doses of antibiotics, researchers divided the dish into sections and saturated them with various doses of medication. The outermost rims of the dish were free of any drug. The next section contained a small amount of antibiotic—just above the minimum needed to kill the bacteria—and each subsequent section represented a 10-fold increase in dose, with the center of the dish containing 1,000 times as much antibiotic as the area with the lowest dose.
Over two weeks, a camera mounted on the ceiling above the dish took periodic snapshots that the researchers spliced into a time-lapsed montage. The result? A powerful, unvarnished visualization of bacterial movement, death and survival; evolution at work, visible to the naked eye.
The device, dubbed the Microbial Evolution and Growth Arena (MEGA) plate, represents a simple, and more realistic, platform to explore the interplay between space and evolutionary challenges that force organisms to change and adapt or die, the researchers said.
“We know quite a bit about the internal defense mechanisms bacteria use to evade antibiotics but we don’t really know much about their physical movements across space as they adapt to survive in different environments,” said study first author Michael Baym, a research fellow in systems biology at HMS.
The researchers caution that their giant petri dish is not intended to perfectly mirror how bacteria adapt and thrive in the real world and in hospital settings, but it does mimic more closely the real-world environments bacteria encounter than traditional lab cultures. This is because, the researchers say, in bacterial evolution, space, size and geography matter. Moving across environments with varying antibiotic strengths poses a different challenge for organisms than they face in traditional lab experiments that involve tiny plates with homogeneously mixed doses of drugs.
Through the observations of this experiment the scientists were able to gather some key insights about the behaviour of bacteria exposed to increasing doses of a drug, including,
Bacteria spread until they reached a concentration (antibiotic dose) in which they could no longer grow.
At each concentration level, a small group of bacteria adapted and survived. Resistance occurred through the successive accumulation of genetic changes. As drug-resistant mutants arose, their descendants migrated to areas of higher antibiotic concentration. Multiple lineages of mutants competed for the same space. The winning strains progressed to the area with the higher drug dose, until they reached a drug concentration at which they could not survive.
Progressing sequentially through increasingly higher doses of antibiotic, low-resistance mutants gave rise to moderately resistant mutants, eventually spawning highly resistant strains able to fend off the highest doses of antibiotic.
Ultimately, in a dramatic demonstration of acquired drug resistance, bacteria spread to the highest drug concentration. In the span of 10 days, bacteria produced mutant strains capable of surviving a dose of the antibiotic trimethoprim 1,000 times higher than the one that killed their progenitors. When researchers used another antibiotic—ciprofloxacin—bacteria developed 100,000-fold resistance to the initial dose.
Initial mutations led to slower growth—a finding that suggests bacteria adapting to the antibiotic aren’t able to grow at optimal speed while developing mutations. Once fully resistant, such bacteria regained normal growth rates.
The fittest, most resistant mutants were not always the fastest. They sometimes stayed behind weaker strains that braved the front-lines of higher antibiotic doses.
Richard Dawkins in his facebook page describes this as a a powerful demonstration of how quickly bacteria can develop resistance to antibiotics.
Source – Harvard Medical School Website